Herniated Disc Treatment in Fort Wayne
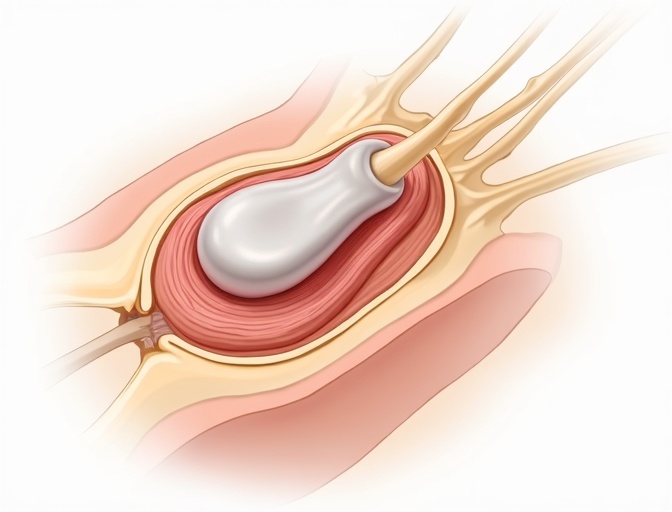
A herniated disc happens when the gel-like center pushes through a crack in the tough outer layer, potentially pressing on nearby nerves. Before considering surgery, we evaluate whether conservative treatments like physical therapy, anti-inflammatory medications, and epidural injections can resolve your symptoms. Most herniated discs improve naturally over 6-12 weeks—about 80-90% of patients avoid surgery. When conservative care doesn't provide adequate relief after 8-12 weeks, or when you have progressive weakness, minimally invasive surgical options offer proven results. Microdiscectomy has 90-95% success rates for leg pain relief, with most patients returning to normal activity within 4-6 weeks. Care is available in Fort Wayne, Indiana.
Treatment Options Comparison
| Treatment | Best For | Recovery Time | Success Rate |
|---|---|---|---|
Conservative Care PT, meds, injections | Acute symptoms, first 6-12 weeks | 6-12 weeks | 80-90% |
Microdiscectomy Standard surgical approach | Failed conservative care, persistent leg pain | 4-6 weeks | 90-95% |
Endoscopic Discectomy Ultra-minimally invasive | Select herniations, suitable anatomy | 2-4 weeks | 85-95% |
Success rates refer to significant improvement in leg pain. Individual results vary based on specific condition and patient factors.
Conservative Treatment
Conservative care is the first line of treatment for most herniated discs. Many patients experience significant improvement without surgery.
Activity Modification
Temporary restrictions on lifting, bending, and prolonged sitting to allow healing
NSAIDs and Medications
Anti-inflammatory drugs and nerve pain medications to reduce symptoms
Physical Therapy and Core Strengthening
Targeted exercises to support the spine and improve flexibility
Epidural Steroid Injections
Targeted injections to reduce inflammation around compressed nerves
Heat and Ice Therapy
Application of heat or cold to manage pain and inflammation
Manual Therapy
Chiropractic care and massage to improve mobility and reduce muscle tension
When to Consider Surgery
Surgery is considered when conservative treatments haven't provided adequate relief after 6-12 weeks, or when there are serious neurological symptoms requiring immediate attention.
Objective Triggers for Surgery
- Progressive neurological deficit
- Intractable radicular pain after 6-12 weeks
- Cauda equina syndrome (emergency)
- Significant functional impairment
Why Greenberg Spine
Our advanced approach combines:
- Robotics for precise navigation
- Endoscopic techniques for minimal tissue damage
- Motion-preserving philosophy
- Outpatient focus for faster recovery
Related Procedures
Recovery Expectations
Conservative Treatment
Most patients improve within weeks with proper conservative care. The body's natural healing process can resolve many disc herniations.
Weeks 1-2
Pain management and gentle movement
Weeks 3-6
Physical therapy and gradual activity increase
Weeks 6-12
Return to normal activities and strengthening
Surgical Recovery
Minimally invasive surgery often provides immediate relief of leg pain, with recovery measured in days to weeks rather than months.
Days 1-7
Rest and wound healing, walking encouraged
Weeks 2-4
Gradual increase in activity, physical therapy begins
Weeks 4-12
Return to work and normal activities
Frequently Asked Questions
Will my herniated disc heal on its own?
Many herniated discs improve naturally over 6-12 weeks. The body's immune system can resorb herniated disc material, and symptoms often resolve with conservative treatment. About 80-90% of patients avoid surgery. However, if you have progressive weakness, severe pain lasting beyond 8-12 weeks, or bowel/bladder dysfunction, surgical evaluation is appropriate.
How do I know if I need surgery for my herniated disc?
Surgery becomes reasonable when: conservative treatment fails after 6-12 weeks, you have progressive leg weakness (foot drop), there's significant functional impairment affecting work or daily life, or you have cauda equina syndrome (bowel/bladder dysfunction—this is urgent). The decision depends on your specific symptoms, MRI findings, and how the condition affects your life.
What's the difference between microdiscectomy and endoscopic discectomy?
Both remove herniated disc material pressing on nerves. Microdiscectomy uses a small incision (2-3cm) with microscope visualization—it's the time-tested standard with 90-95% success rates. Endoscopic discectomy uses an even smaller incision (7-8mm) with camera visualization, potentially allowing faster recovery. Not all herniations are suitable for endoscopic approach. The choice depends on herniation location, size, and your anatomy.
Can a herniated disc come back after surgery?
Recurrence happens in about 5-10% of patients, usually within the first year. We remove only the herniated portion of the disc, so there's remaining disc material that could potentially herniate again. Risk factors include smoking, obesity, heavy lifting, and the size of the original herniation. Proper post-op activity modification and core strengthening reduce this risk.
How long until I can return to work after herniated disc surgery?
Desk work: typically 2-3 weeks. Light physical work: 4-6 weeks. Heavy lifting or labor: 8-12 weeks. Endoscopic approaches may allow faster return. The limiting factor is usually sitting tolerance and the need to avoid prolonged flexion while the surgical site heals. Most patients notice immediate leg pain improvement but need time for incision healing and strength recovery.
Should I get an MRI right away for my herniated disc?
MRI is most useful when it would change your treatment plan. I typically order imaging if: symptoms persist beyond 6-8 weeks despite conservative care, you have progressive weakness, there are red flags like bowel/bladder changes, or we're considering injections or surgery. Early MRI for mild symptoms often creates unnecessary anxiety without changing initial treatment, which is conservative care regardless of MRI findings.
Related Topics
Learn more about related conditions and treatments
Ready to Find Relief from Your Herniated Disc?
Schedule a consultation with Dr. Greenberg to explore your treatment options and get back to living pain-free.
Medical Disclaimer: This information is for educational purposes and should not replace professional medical advice. Always consult with a qualified healthcare provider for proper diagnosis and treatment recommendations. Individual results may vary.
Source: American Association of Neurological Surgeons (AANS) and North American Spine Society (NASS) clinical guidelines.
